Heading picture taken by Ed Uthman.
|
When your immune system comes into contact with a cell that has an HLA marker that is different than the markers on your cells your immune system will target the foreign cells for destruction.
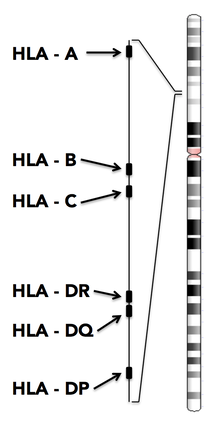
Each of your cells presents a combination of more than 200 HLA markers. However, some of these markers are more important than others in terms of immune system recognition. There are 6 main HLA markers that the immune system uses to target foreign cells. These HLA markers are called HLA-A, HLA-B, HLA-C, HLA-DR, HLA-DP, and HLA-DQ. These HLA markers are coded for by genes on chromosome 6. Genes code for proteins. The gene for HLA-A codes for an HLA-A protein. What makes this more complicated is that there are different versions of the HLA-A gene that code for different versions of the HLA-A protein. This is what makes it so that one person's HLA-A marker might be different than another person's HLA-A marker. There are 59 known versions of the HLA-A gene, 118 versions of the HLA-B gene, and 124 versions of the HLA-C gene. With this much variation in just these three markers it can be very difficult to find a perfect match. Inheritance of HLA markers |
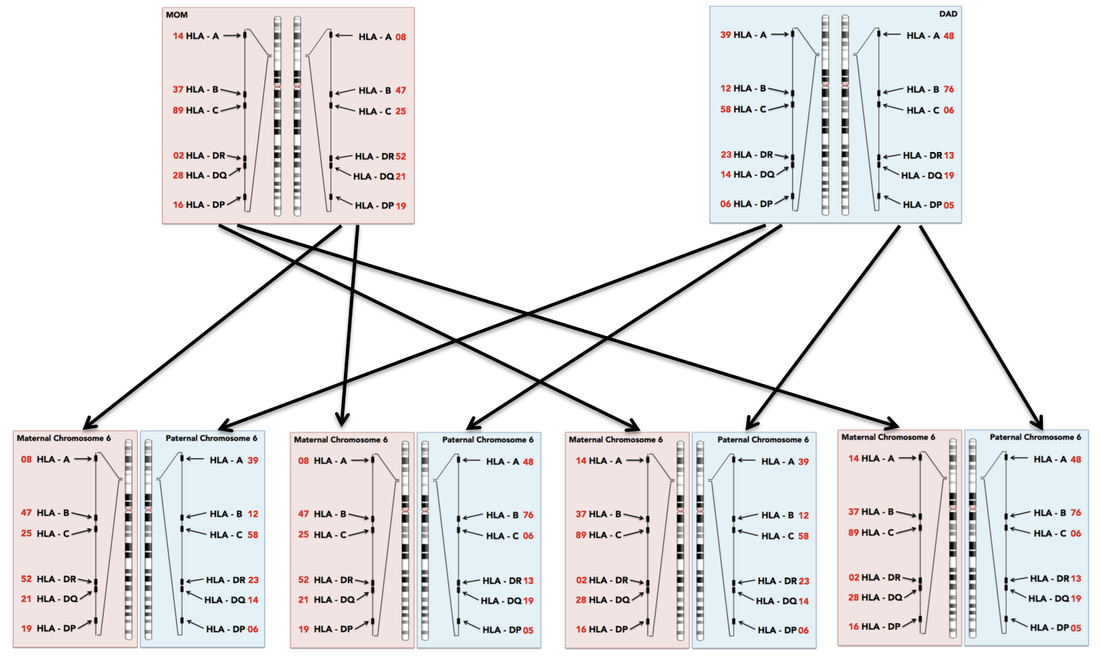
When looking for a match the first place a doctor will check is with the patients siblings. As HLA markers are coded for in DNA, and DNA is passed down from parents to children, siblings have a 25% chance of having the same HLA markers.
As the main HLA markers are all on the same chromosome they are all inherited together. You have two copies of chromosome 6, one from your mom and one from your dad. This means there are 12 main HLA markers that you inherit from your parents, 6 from mom and 6 from dad.
As all 6 genes are on the same chromosome we only have to look at one of the markers to see how the genes are inherited.
As the main HLA markers are all on the same chromosome they are all inherited together. You have two copies of chromosome 6, one from your mom and one from your dad. This means there are 12 main HLA markers that you inherit from your parents, 6 from mom and 6 from dad.
As all 6 genes are on the same chromosome we only have to look at one of the markers to see how the genes are inherited.
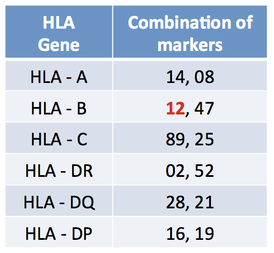
In the diagram above all the parental genes are listed. Each gene is given a number to show what version of that gene the parent has. If we look at HLA-A we can see that the mom has version 14 and version 08. On the other hand, dad has version 39 and version 48. The children can inherit any combination of these as long as they have one from mom and one from dad. Looking at just HLA-A, the children will have either (08,39), (08,48), (14,39) or (14,48). There are four combinations so there is a 1/4 chance of getting each combination.
Matching HLA markers
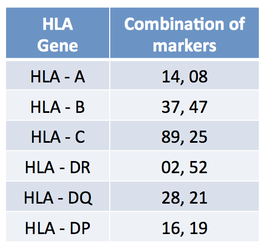
A perfect match occurs when the donor and the patient have the exact same versions of each of the 6 markers. Because each person has two genes for each marker a perfect match would be identical for all 12 markers. See the table below showing the mother's combination of markers from the example above.
|
Mother's markers for all 6 HLA genes. Notice that she has two markers for each gene (because she has two copies of each chromosome) so there are 12 markers total.
|
A person with the markers shown below would be an 11/12 match to the mother as they have 11 markers that are identical and one marker (HLA-B12) different.
|
About 30% of people can find a match from a family member. This means that about 70% of people need to find a match from the national donor registry (Be The Match). The lowest match allowable from Be The Match is 6 out of 8 HLA markers. The markers used by Be The Match are HLA-A, HLA-B, HLA-C, and HLA-DR. Some doctors and organizations require higher matches, such as 8/8, or they look at more markers, for example they could look for an 8/10 match by also looking at HLA-DQ or a in which case they may looks for a 9/12 match if they also looked at HLA-DP.
How your ethnicity affects your chance of finding a match...
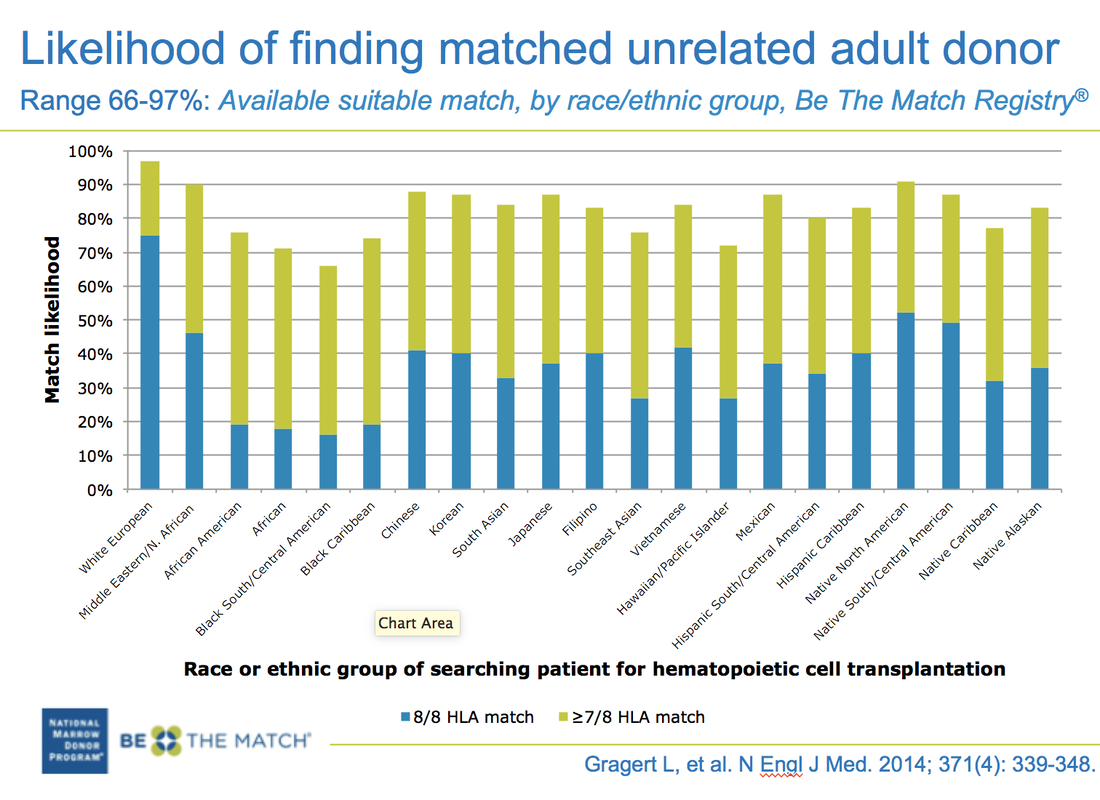
HLA genes are inherited in the same way that ethnicity is inherited. This means that you are more likely to find a match that has your same ethnicity. Caucasian people have fewer HLA markers in the population, so there is less variation between individuals. This makes the chance of finding a match higher for caucasian people than for people of other ethnicities. People with mixed ethnicity are the hardest to match because there is much more variation in their HLA markers and the chance of finding the same combination of markers is more rare. As mixed ethnicity people are becoming more and more common it is becoming harder and harder to find people good HLA matches.
Below is a chart showing the probability of finding a match for adults of different ethnicities.
Below is a chart showing the probability of finding a match for adults of different ethnicities.
Transplants problems: graft vs. host disease
Your immune system uses HLA markers to determine if a cell is supposed to be in your body or not. If the HLA marker is not recognized then the immune system will kill the invading cell. T cells are a type of white blood cell that read HLA markers and destroy foreign cells.
When someone get a bone marrow donation they are getting the immune system of the donor. The transplanted cells (the graft) contain B cells, T cells, red blood cells, and platelets in addition to the stem cells that will form all these cells. The donated T cells will travel around the recipient's body, looking for HLA markers that they do not recognize. If the patient and donor are not a perfect match then the donated T cells will think that the patient's cells are foreign. The donated cells will destroy the patients cells. This immune response by the donated cells on the patient cells makes the patient ill.
The more markers that are mismatched the more likely it is that the patient will experience graft vs. host disease.
When someone get a bone marrow donation they are getting the immune system of the donor. The transplanted cells (the graft) contain B cells, T cells, red blood cells, and platelets in addition to the stem cells that will form all these cells. The donated T cells will travel around the recipient's body, looking for HLA markers that they do not recognize. If the patient and donor are not a perfect match then the donated T cells will think that the patient's cells are foreign. The donated cells will destroy the patients cells. This immune response by the donated cells on the patient cells makes the patient ill.
The more markers that are mismatched the more likely it is that the patient will experience graft vs. host disease.
Proudly powered by Weebly